Latest Article:
Bionique’s Research Presented in Advances in Biotechnology & Microbiology
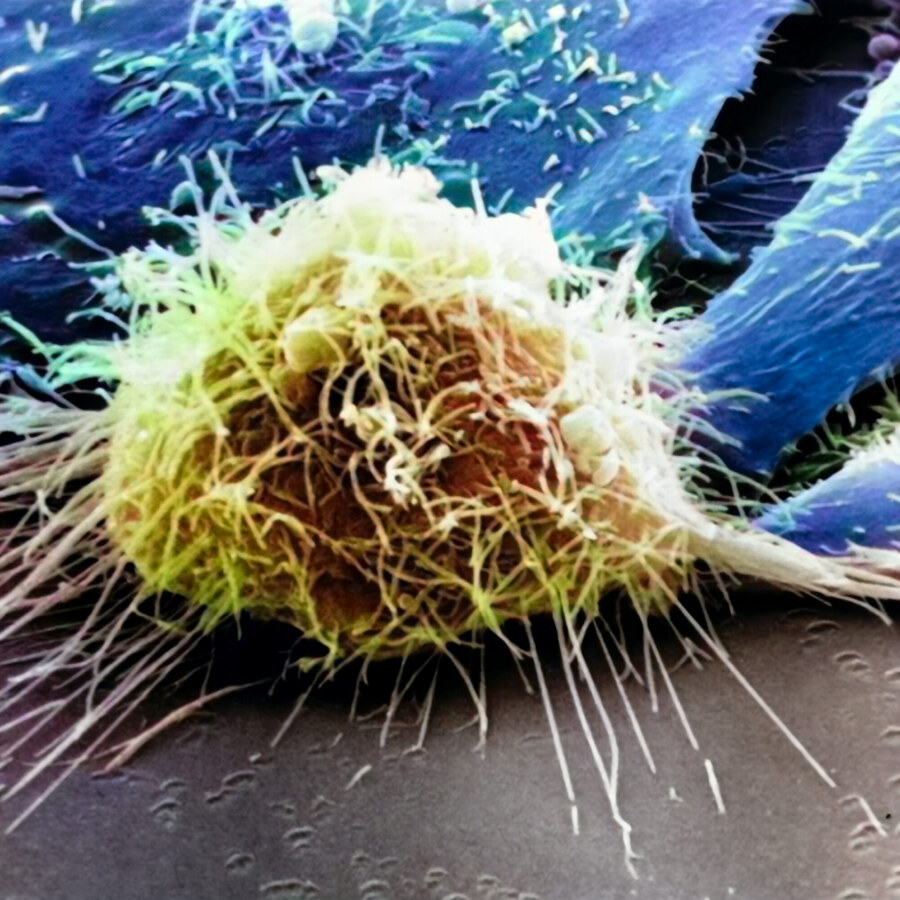
Bionique’s Research Presented in Advances in Biotechnology & Microbiology Research conducted at Bionique Testing Laboratories was published in an article that studies the impact of aerobicity on colony growth of various mollicutes, including mycoplasma, on agar in order to confirm the optimal oxygen content for colony growth for isolation of mycoplasma from cell cultures for […]
Read ArticleBionique Appoints Gladis Zamparo as new Chief Executive Officer
Gladis Zamparo will lead the commercial testing organization in its next phase of growth and innovation November 16, 2020 — Bionique Testing Laboratories, Inc. is thrilled to announce that it has selected Gladis Zamparo as its next CEO effective November 16, 2020. Zamparo has spent two decades in global organizations driving change through innovative solutions, […]
Read ArticleBionique in Association with ThermoFisher and American Pharmaceutical Review Present: Key Considerations for Implementing Rapid Microbial Methods for Mycoplasma Detection.
Bionique in Association with ThermoFisher and American Pharmaceutical Review Present: Key Considerations for Implementing Rapid Microbial Methods for Mycoplasma Detection. This white paper explains the importance of demonstrating product-specific suitability, defining representative sample, consistent sampling protocols, accommodating volume and turnaround time constraints, and the need to establish equivalence. Rapid microbial methods are increasingly being used […]
Read ArticleBionique to Expand After Acquisition by Asahi Kasei Medical
Bionique to Expand After Acquisition by Asahi Kasei Medical SARANAC LAKE, NY – December 15, 2021 – Bionique Testing Laboratories LLC (Bionique; www.bionique.com), a global leader in mycoplasma testing services for the biologics and life-sciences industries, announced today that it has been 100% acquired by a subsidiary of Japan-based healthcare pioneer Asahi Kasei Medical Co., […]
Read ArticleResearch, References, and Regulatory Guidelines
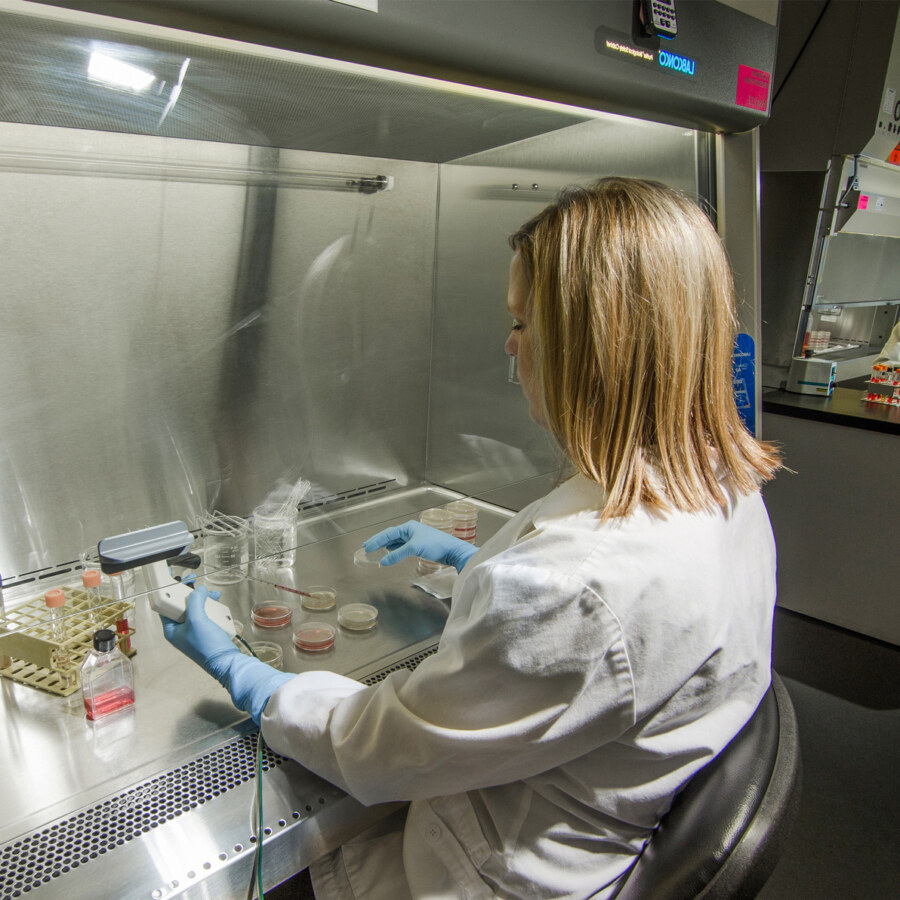
At Bionique, it’s crucial to have a thorough understanding of mycoplasma and its implications in your products. We’ve compiled a list of some of the best resources to learn more about mycoplasma.
Read ArticleWant to read the latest about Bionique?
Read our latest news and announcements.